Step 2 CS Blue Sheet Hypertension
Hypertension is an extremely common disease found in the medical practice in all settings. Recognizing the most common secondary effects on the human body caused by the higher levels of blood pressure in this patients is the most important task. Medication compliance and correct use are crucial as well, and the identification of possible side effects from anti-hypertensive drugs should always be pursued. Assessment and management of cardiovascular risk factors (hypertension, smoking, diabetes, hyperlipidemia, etc.) should be done and corrected in all patients.
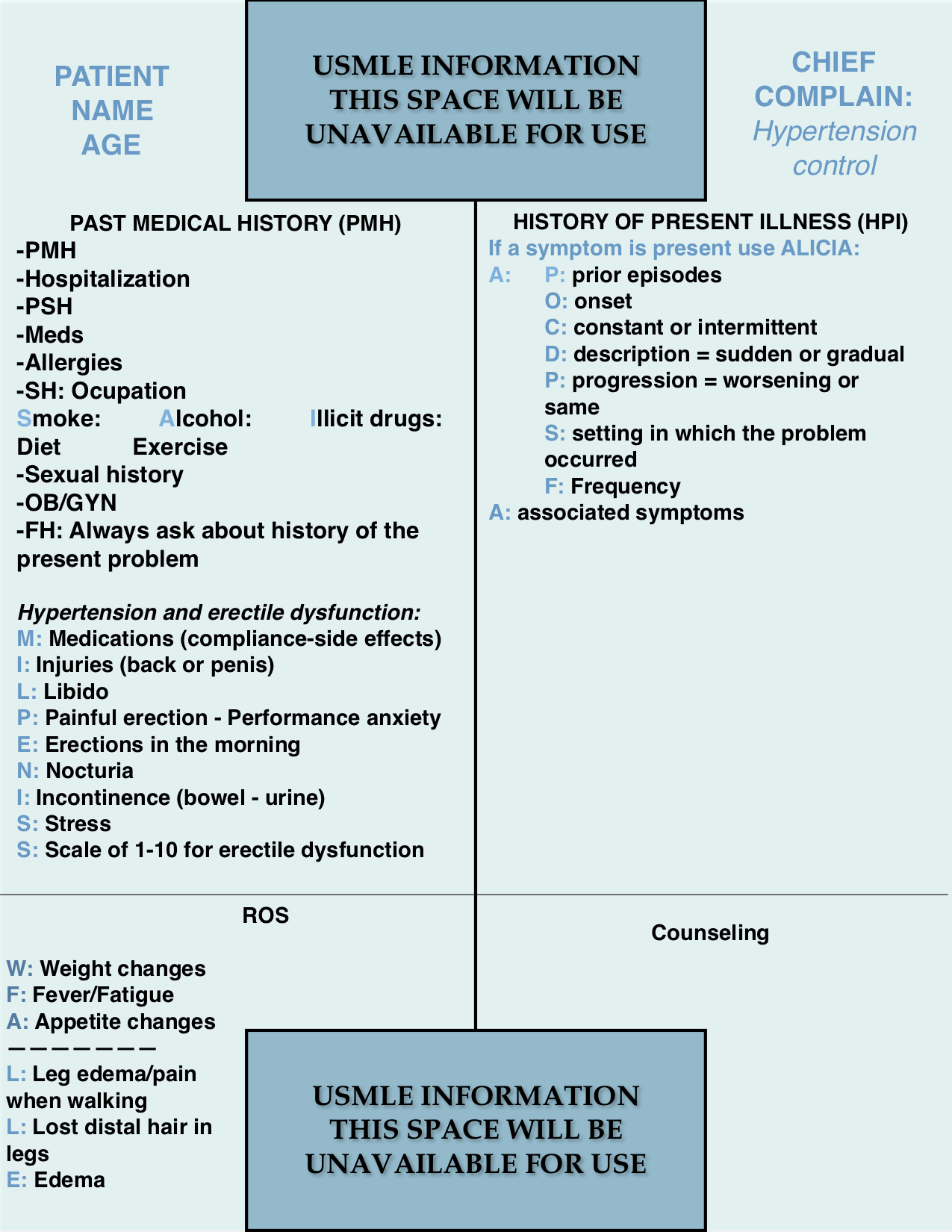
Let us review the suggested blue sheet, physical exam, diagnostic studies, and differential diagnosis needed to be done for addressing hypertension in USMLE Step 2 CS exam:
IMPORTANT ASPECTS OF THE PAST MEDICAL HISTORY:
The most important aspect of the past medical history is the assessment of the duration of hypertension, consequences, cardiovascular risks and events, medication compliance and correct use, medication side effects, and identification of possible secondary causes of hypertension (Chronic Kidney Disease, hyperaldosteronism, etc.).
The mnemonic (MIL PENISS) is a good tool for screening for erectile dysfunction and medication compliance. Use the entire mnemonic only if there is erectile dysfunction, otherwise, it is not necessary.
IMPORTANT ASPECTS OF THE HISTORY OF PRESENT ILLNESS:
Ask about any symptom that may be present in the patient and use the usual mnemonics for HPI.
IMPORTANT ASPECTS OF THE REVIEW OF SYSTEMS:
Screen for constitutional symptoms (WFA) and use the mnemonic LLE for asking about edema, leg pain while walking (claudication), lost distal leg hair (peripheral arterial disease), and distal ulcerations.
PHYSICAL EXAMINATION:
1. HEENT/Neck:
- Eyes: fundoscopy.
- Neck: thyroid gland assessment, carotid pulses palpation and auscultation for bruits, JVD.
2. Lungs:
- Auscultation.
3. Cardiovascular:
- Auscultation.
- PMI.
4. Abdomen:
- Inspection.
- Palpation for hepatomegaly.
- Auscultation for abdominal bruits (renal arterial stenosis).
5. Extremities:
- Inspection for lost distal hair, ulcerations, edema.
- Palpation of peripheral pulses and edema.
6. Neurologic (if pertinent, for example when there is a history of cerebrovascular disease):
- Motor.
- Sensory.
- DTR’s.
WORKUP (focused on the clinical suspicion):
- Genital exam (erectile dysfunction).
- CBC.
- Electrolytes, glucose, HbA1C.
- BMP or CMP.
- Lipid profile.
- U/A (Urinalysis).
- TSH, T4.
- Electrocardiogram ECG.
- Echocardiogram when needed.
- Ankle brachial index (ABI) for peripheral arterial disease.
- Doppler US penis.
- Aldosterone, testosterone, calcium, prolactin, etc: for secondary hypertension.
DIFFERENTIAL DIAGNOSIS:
Primary (essential) Hypertension.
Secondary hypertension:
- Diabetes complications (diabetic nephropathy).
- Polycystic kidney disease.
- Glomerular kidney disease.
- Renovascular hypertension.
- Cushing syndrome.
- Aldosteronism.
- Pheochromocytoma.
- Thyroid problems: both hyperthyroidism and hypothyroidism can cause hypertension.
- Hyperparathyroidism.
- Coarctation of the aorta.
- Sleep apnea.
- Obesity.
- Pregnancy (pregnancy-induced hypertension or preeclampsia).
- Medications: NSAIDs, contraceptives, antidepressants, etc.
Consequences of hypertension:
- Erectile dysfunction.
- Peripheral arterial disease.
- Congestive heart failure.
- Coronary arterial disease (eg. MI).
- Hypertensive Retinopathy.
- Hypertensive Nephropathy.
- Cerebrovascular disease (eg. stroke).
- Carotid atherosclerosis.
We hope that this post can help you better understand how to handle a case of hypertension in your exam. Please, feel free to contact us should you have any comment or question by using the comments section below. Good luck with your studies.
- Aortic Stenosis Severity Classification - 09/22/2020
- Carboplatin (Paraplatin) - 04/07/2019
- How to test for Vitamin D deficiency? - 09/29/2018