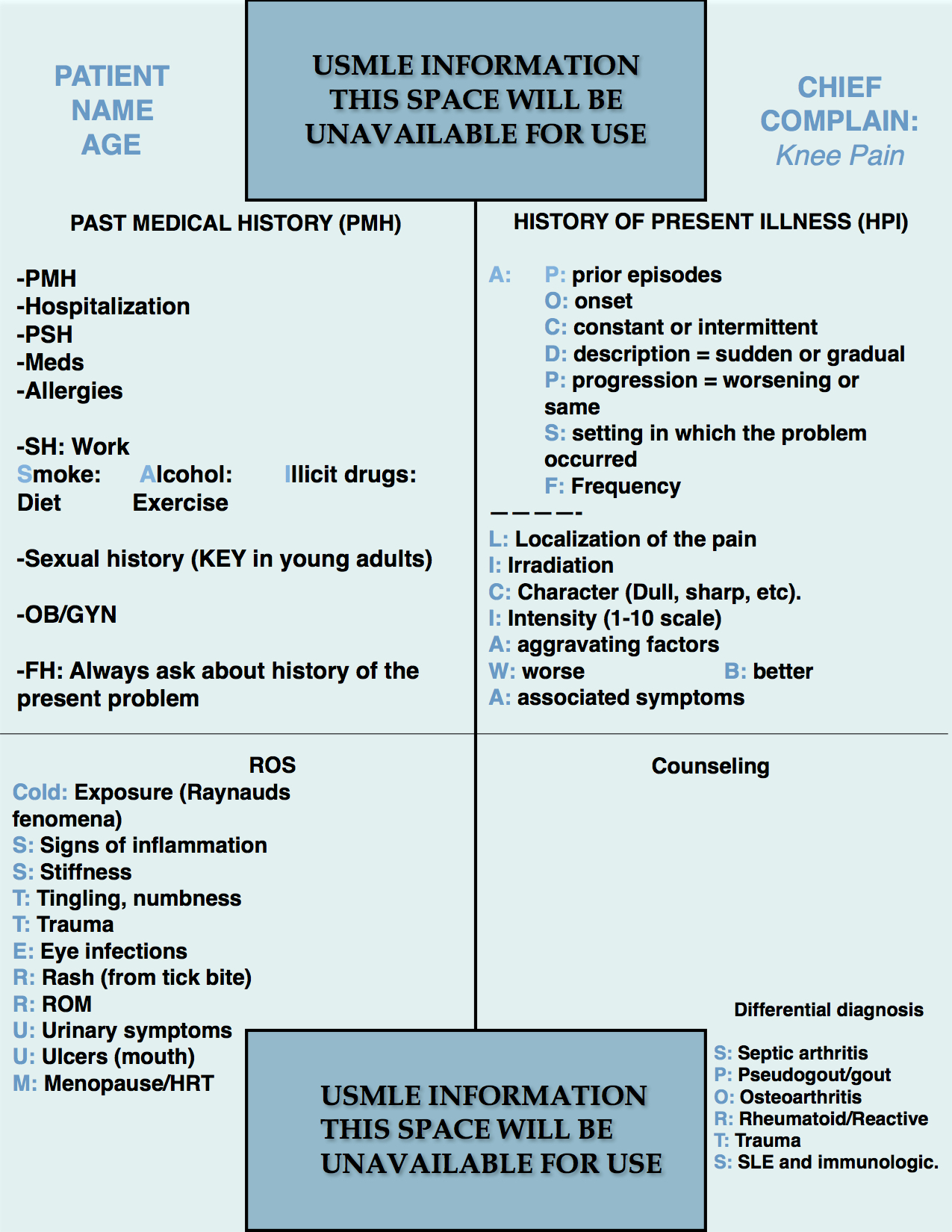
Step 2 CS Blue Sheet Knee Pain Case:
Knee pain is a very common presenting symptom in medicine and the USMLE exams. Let us review the suggested blue sheet, physical exam, diagnostic studies, and differential diagnosis needed to be done for addressing knee pain in USMLE Step 2 CS exam:
Key considerations for a knee pain case:
- Traumatic or activity-related lesions are the most common cause in young adults.
- Asking about the patient’s sexual history to identify risk factors for sexually transmitted diseases (STD’s) is crucial since they are related to joint pain:
- Gonococcal Arthritis is the most common cause of septic arthritis in the U.S. (1)
- Reactive arthritis usually occurs after a gastrointestinal (salmonella, dysentery, food poisoning) or genitourinary infection (chlamydia is the major one). Remember the triad of reactive arthritis: non-gonococcal urethritis, conjunctivitis, and arthritis. (2)
- All acutely inflamed joints need diagnostic arthrocentesis.
MNEMONIC FOR KNEE PAIN (AND ANY OTHER JOINT PAIN):
Write just the initial letters on your blue sheet, then make notes depending on the information given by the SP (standardized patient).
Cold: Ask if exposure to cold provokes changes in the coloration of the fingers from white (ischemia), blue (cyanosis), and then red (rubor) consistent with Raynaud’s phenomena.
S: Signs of inflammation (swelling, erythema, warmth, pain).
S: Stiffness (morning stiffness). Usually, the magic number is one hour, which means that if a patient has morning stiffness more than one hour, one should look for an inflammatory joint disorder such as rheumatoid arthritis.
T: Tingling, numbness, weakness (usually you may ask them together) to evaluate for nervous and muscular compromise.
T: Trauma and recent activity.
E: Eye infections (reactive arthritis has conjunctivitis).
R: Rash – tick bite (Lyme’s disease).
R: Range of motion to evaluate for possible stiffness and decrease mobility of the joint.
U: Urinary symptoms (urethritis in reactive arthritis).
U: Ulcers in the mouth (SLE).
M: Menopause/Hormone replacement therapy (risk for osteoporosis and pathologic fractures) and other medications such as steroids.
PHYSICAL EXAMINATION:
1. HEENT:
Eye inspection (for conjunctivitis).
Mouth inspection (for ulcers or other lesions.
2. Lungs:
Auscultation.
3. Heart:
Auscultation.
4. Extremities:
Inspection (focused on the knee unless there is suspicion of compromise of other joints).
Palpation of both knees with compression of the patella (painful in patellar disorders such as patellar fracture, patellofemoral syndrome).
Range of motion of both knees and hips.
Knee-specific tests:
- Valgus/Varus stress test: for medial and lateral collateral ligament lesions.
- Lachman or Drawer test: To assess for lesions of the anterior cruciate ligament (anterior laxity) and posterior cruciate ligament (posterior laxity).
- McMurray test: for assessment of meniscal lesions.
Source: Tests For Examination Of The Knee – Everything You Need To Know – Dr. Nabil Ebraheim (youtube).
DIFFERENTIAL DIAGNOSIS:
The mnemonic “SPORTS” can help remembering the most important differential diagnosis to bear in mind.
- S: Septic arthritis.
- P: Pseudogout and gout.
- O: Osteoarthritis.
- Rheumatoid arthritis, reactive arthritis.
- Trauma: fractures, medial or lateral collateral ligament lesions, anterior or posterior cruciate ligament lesions, meniscal lesions or fractures, patellar fractures, hematomas, etc.
- S: Systemic lupus erythematosus, sacs in the knee such as the posterior knee pain caused by a rupture of a Baker’s cyst rupture.
WORKUP:
- Pelvic exam when appropriate.
- Infection: CBC with differential, blood culture, urinalysis, urethral culture.
- Arthrocentesis with synovial fluid cytology, crystals, gram stain, culture and sensitivity (C/S).
- Immunologic tests: ANA, rheumatoid factor, anti-dsDNA, anti-CCP, etc.
- X-ray of the knee.
- MRI of the knee (key for ligament and meniscal lesions).
References:
- Gonococcal Arthritis – Medscape.
- Stavropoulos, P.G., Soura, E., Kanelleas, A., Katsambas, A. Antoniou, C. (2015), Reactive Arthritis. J Eur Acad Dermatol Venereol, 29: 415–424. doi:10.1111/jdv.12741. [Pubmed]
We hope that this post can help you better understand how to handle a knee pain case in your exam. Please, feel free to contact us should you have any comment or question by using the comments section below. Good luck with your studies.
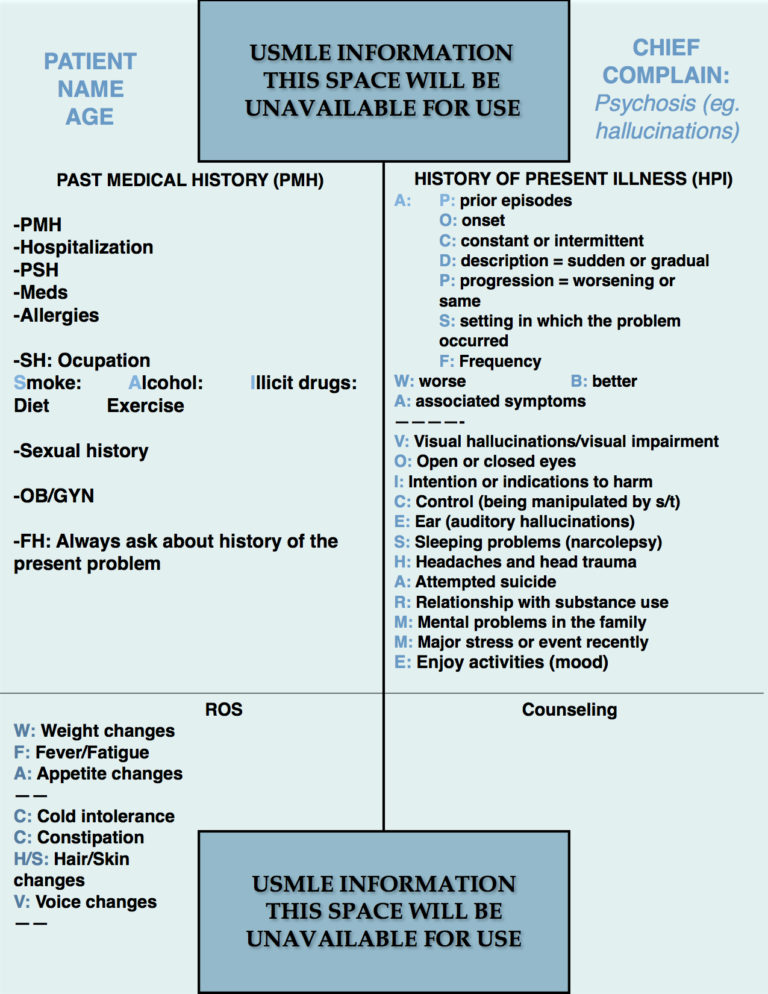
- Step 2 CS Blue Sheet Psychosis - 03/23/2018
- Step 2 CS Blue Sheet Memory Loss/Forgetfulness - 03/23/2018
- Step 2 CS Blue Sheet Shortness of Breath - 03/13/2018