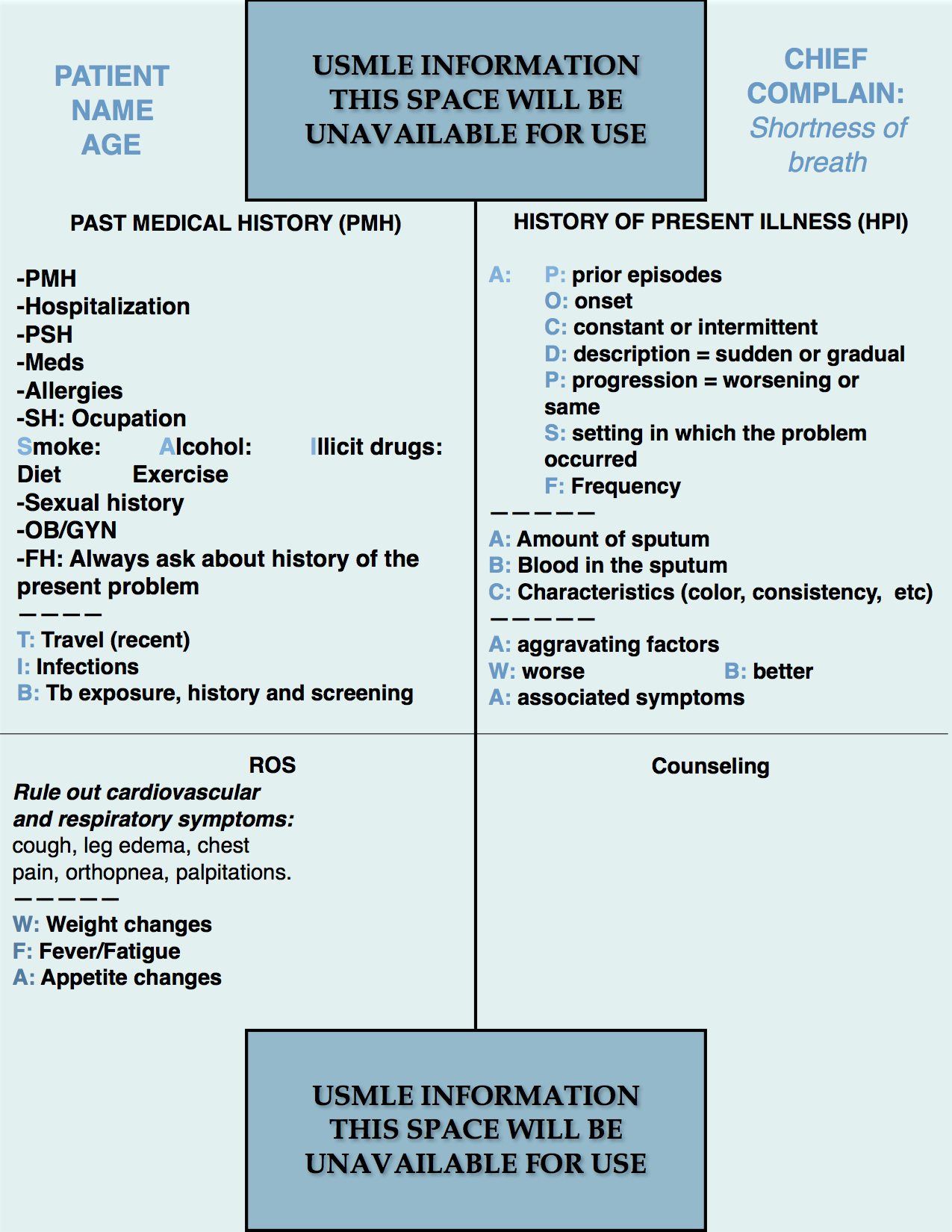
Step 2 CS Blue Sheet Shortness of Breath Case:
Shortness of breath (dyspnea) is a common presenting symptom in the medical practice and it is highly tested in the USMLE exams. Let us review the suggested blue sheet, physical exam, diagnostic studies, and differential diagnosis needed to be done for addressing dyspnea or shortness of breath in USMLE Step 2 CS exam:
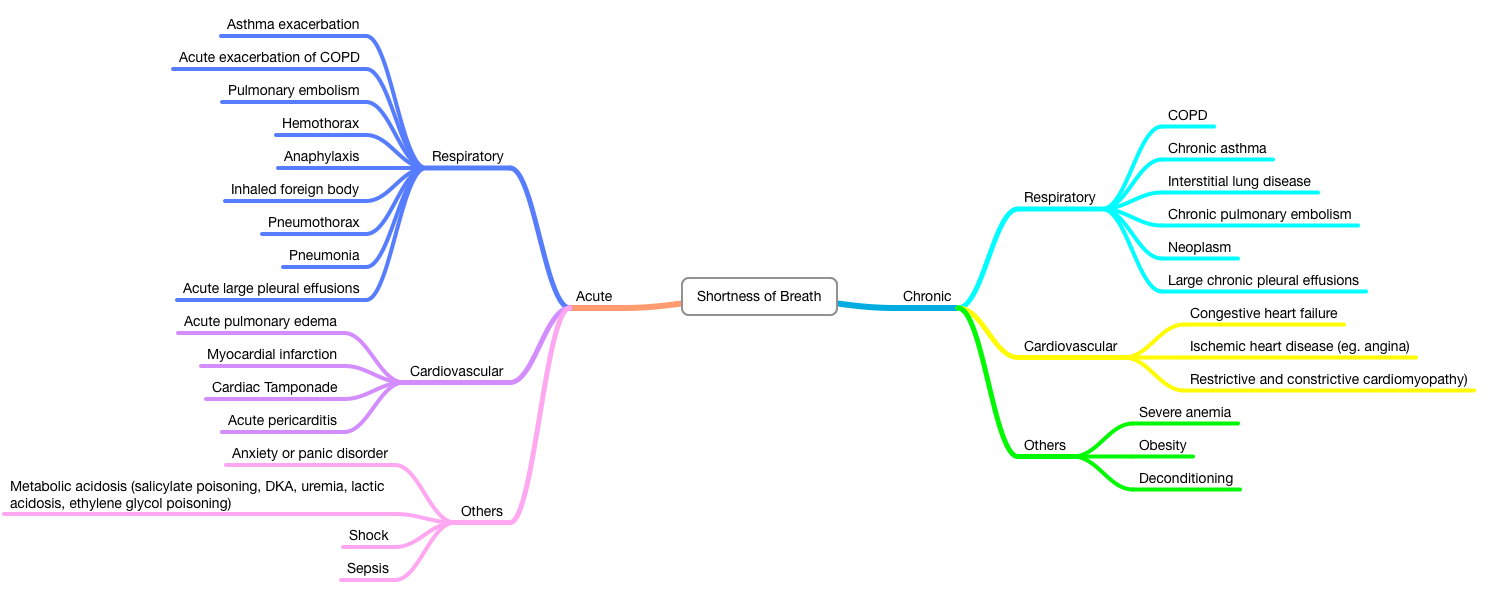
The causes of shortness of breath can be divided into 3 groups: respiratory, cardiovascular and other causes. Therefore, it is wise to focus the history and physical exam mostly on the cardiovascular and respiratory causes. Let’s review the important consideration for a shortness of breath case.
IMPORTANT ASPECTS OF THE PAST MEDICAL HISTORY:
The PMH needs attention mostly in the identification of risk factors and baseline disorders. For example, if a patient has a history of asthma, one would be required to rule out a possible asthmatic exacerbation. A patient with a history of angina and/or myocardial infarction would be more likely to develop heart failure that could cause shortness of breath. The TIB mnemonic used in many cases can help us to identify important risk determinants for infection such as recent travel, upper respiratory infections previous an episode of pneumonia, or exposure or risk factors for tuberculosis.
IMPORTANT ASPECTS OF THE HISTORY OF PRESENT ILLNESS:
The history of present illness would use the mnemonic ABC added to the conventional mnemonic used for cases without pain as the presenting symptom. The ABC mnemonic stands for:
- A: Amount of sputum: usually described as a teaspoon (5 ml), a tablespoon (15 ml) or a cup (250 ml).
- B: Blood in the sputum.
- C: Characteristics where color, consistency, and content are the most important features.
PHYSICAL EXAMINATION:
1. HEENT/Neck:
- Eyes: look for pallor (anemia).
- Neck: Inspect the neck for jugular veins congestion, and auscultate the carotid arteries for signs of stenosis (atherosclerosis).
2. Lungs:
- Inspection.
- Palpation (fremitus).
- Percussion.
- Auscultation (the patient may move the chest wall simulating an inspiration without air movement as a sign of decreased or absent breath sounds in the area of auscultation.
3. Cardiovascular:
- Palpation for thrills and the point of maximal impulse (PMI).
- Auscultation.
4. Abdomen:
- Palpation for hepatomegaly if required (as when there is suspicion of hear failure with hepatic congestion).
6. Extremities:
- Inspect for edema and signs of hypoperfusion (eg. lost distal hair in the legs that suggest peripheral arterial disease).
- Palpate for peripheral pulses, calf tenderness, and Homan’s sign (for venous thromboembolism VTE).
WORKUP (focused on the clinical suspicion):
- CBC.
- Comprehensive metabolic panel (CMP).
- C-reactive protein.
- Blood cultures.
- Sputum analysis, gram, and culture.
- Electrocardiogram (EKG or ECG).
- Echocardiogram.
- Chest X-ray.
- D-dimer.
- Brain natriuretic peptide (BNP).
- Chest CT angiography.
- V/Q scan.
DIFFERENTIAL DIAGNOSIS:
We hope that this post can help you better understand how to handle a case of shortness of breath in your exam. Please, feel free to contact us should you have any comment or question by using the comments section below. Good luck with your studies.
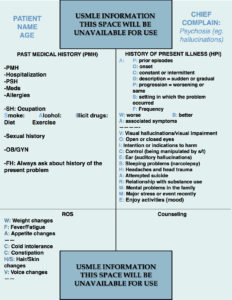
- Step 2 CS Blue Sheet Psychosis - 03/23/2018
- Step 2 CS Blue Sheet Memory Loss/Forgetfulness - 03/23/2018
- Step 2 CS Blue Sheet Shortness of Breath - 03/13/2018