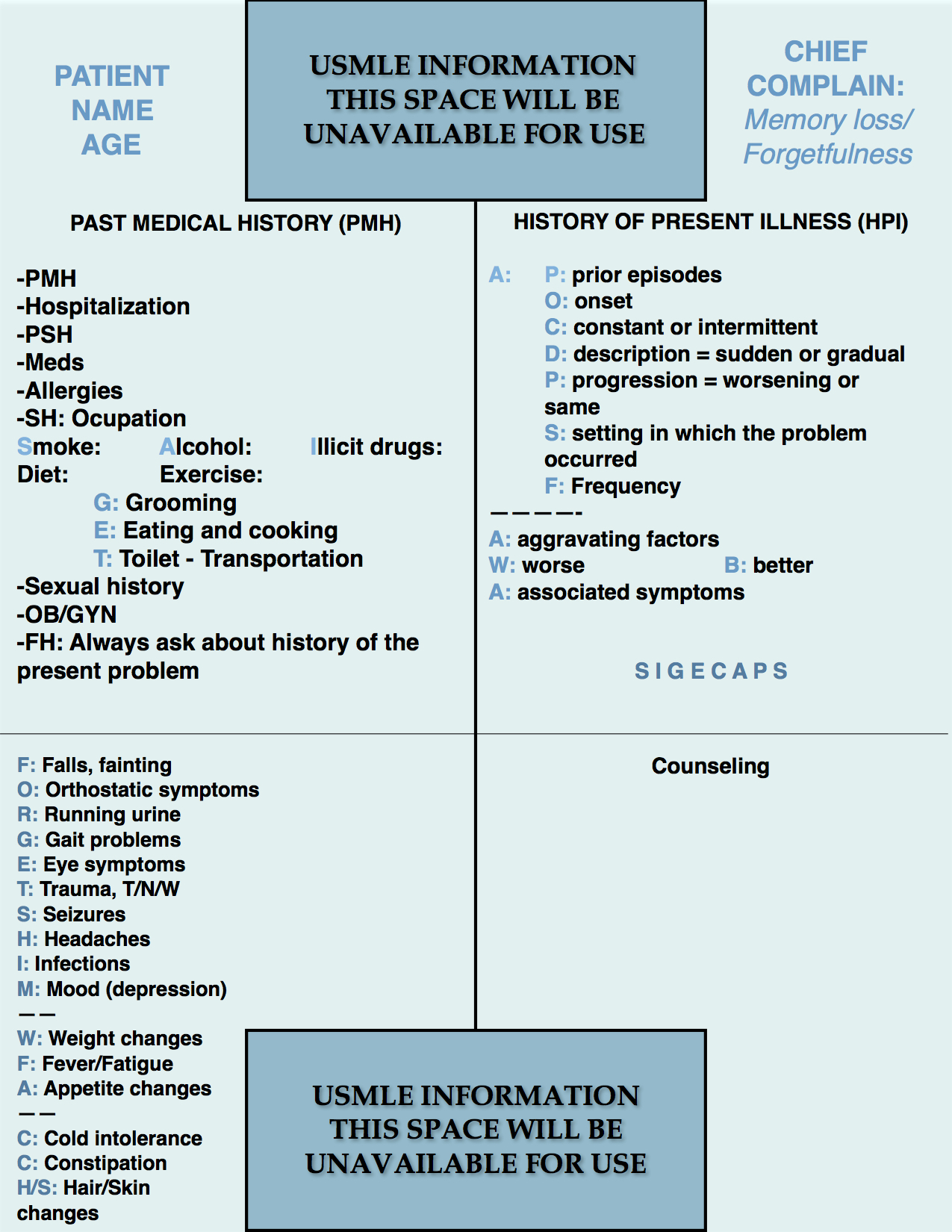
Step 2 CS Blue Sheet Memory Loss/Forgetfulness
Memory loss or forgetfulness is commonly tested on the USMLE Step 2 CS exam. Memory loss if a common complaint in the primary care setting. Elderly patients present with forgetfulness more often than the younger patients, although it can also occur in these patients. In some cases, the family members are the ones who report the origin of this symptom.
Let us review the suggested blue sheet, physical exam, diagnostic studies, and differential diagnosis needed to be done for addressing memory loss in USMLE Step 2 CS exam:
IMPORTANT ASPECTS OF THE PAST MEDICAL HISTORY:
The PMH needs attention mostly in the identification of independence of activities. A patient experiencing memory loss may have dementia or another disorder as a feasible cause of his or her symptoms. Therefore, identification of activities of daily living (ADL’s) is crucial. In our blue sheet, the mnemonic GET helps one to ask about these activities:
- G: Grooming: Showering, dressing, hygiene in general.
- E: Eating: Can the patient eat without assistance. One can also ask about cooking capacity.
- T: Toilet independent use. Transportation: can the patient drive or use transportation means by his or herself.
IMPORTANT ASPECTS OF THE HISTORY OF PRESENT ILLNESS:
The history of present illness should focus on the natural history of the current event, focusing in the chronology of the symptoms, setting, characteristics such as constant memory disturbances (eg. dementia) versus fluctuating forgetfulness (eg. delirium). You can write the mnemonic SIGECAPS for identifying depression as a culprit for the memory impairment (pseudodementia). When you see the mnemonic SIGECAPS you can remind yourself to ask about mood, and if the response is consistent with a low mood, you can continue asking every letter of the mnemonic. Otherwise, it is not necessary to do so.
SIGECAPS:
S: Sleep problems.
I: Lack of interest.
G: Guiltiness.
E: Energy level decreased.
C: Concentration diminished.
A: Appetite changes.
P: Psychomotor retardation.
S: Suicidality (ideation, intention, plan).
IMPORTANT ASPECTS OF THE REVIEW OF SYSTEMS:
The mnemonic FORGETS HIM can aid screening for other possible causes of the patient’s presenting symptoms. It stands for the following:
- F: Falls: As a cause of head trauma and falls as imbalance causing the patient to fall when standing or walking. Fainting can also be assessed for a central nervous system or systemic disorder causing secondary brain injury.
- O: Orthostatic symptoms such as orthostatic hypotension.
- R: Running urine: Urinary incontinence (a patient with normal pressure hydrocephalus can present with the triad of urinary incontinence, gait abnormalities, and dementia).
- G: Gait abnormalities: Differentiate between imbalance and a genuine gait disorder.
- E: Eye problems (double vision, blurred vision, and other eye abnormalities, sequels of CNS problems such as optic neuritis, intracranial hypertension causing papilledema, and others).
- T: Trauma to the head (eg. epidural or subdural hematomas). Use the convenient acronym for identifying nerve disorders “T/N/W” for asking about tingling and numbness for sensory disturbances, and weakness for motor alterations.
- S: Seizures.
- H: Headache: Can be related to vascular dementia (microvascular dementia due to small vessel disease), vasculitis such as Giant Cell Arteritis, infections, intracranial hypertension, etc.
- I: Infections: Acute and chronic infections causing memory loss such as syphilis, HIV-related CNS infections, meningitis, encephalitis, etc.
- M: Mood: Another chance to ask about mood if not done with the SIGECAPS mnemonic.
Screening for constitutional symptoms can be done with the mnemonic W/F/A:
- W: Weight loss or gain.
- F: Fever and fatigue.
- A: Appetite changes.
Screening for thyroid disorders can be accomplished by using the acronym CCH/S:
- C: Cold or heat intolerance.
- C: Constipation or diarrhea.
- H/S: Hair or skin changes such as alopecia and dry skin.
PHYSICAL EXAMINATION:
1. HEENT/Neck:
- Eyes: look for pallor (anemia). Fundoscopy* for papilledema or vascular changes. PERRLA.
- Neck: Inspect the neck for jugular veins congestion, and auscultate the carotid arteries for signs of stenosis (atherosclerosis). Palpate for lymphadenopathy and thyroid gland assessment.
2. Lungs:
- Auscultation.
3. Cardiovascular (more importance when cardiovascular risks are present):
- Palpation for thrills and the point of maximal impulse (PMI).
- Auscultation.
4. Neurologic:
- Cranial nerves 2-12.
- Mental status:
- Orientation: A/O x 3.
- Repetition: 3-word repetition.
- Order: “close your eyes, then clap and open your eyes.”
- Attention or concentration: spell backward the word “magical” or any other word.
- Recall: 3-word recall after 1 min (after doing all the others).
- Motor.
- Sensory.
- DTR’s.
- Gait.
- Cerebellar signs: Romberg and finger-to-nose or heel-to-knee.
* In my opinion, fundoscopy should not be done in an exam such as the USMLE Step 2 CS exam, since the true quality of a fundoscopic examination done without the appropriately dark setting and drug-induced eye dilation. Since it may be scored during the exam, try to do it fast and move on. That is my recommendation.
WORKUP (focused on the clinical suspicion):
- CBC.
- Comprehensive metabolic panel (CMP).
- TSH, T4.
- Vitamin B12.
- VDRL, RPR.
- HIV testing.
- Electrocardiogram ECG.
- Lipid profile.
- Chest X-ray.
- Carotid duplex study.
- MRI or CT scan of the brain.
- Lumbar puncture.
- Electroencephalogram (only for seizure disorders).
DIFFERENTIAL DIAGNOSIS:
- Dementia:
- Alzheimer’s dementia.
- Vascular dementia.
- Pseudodementia (depression and/or hypothyroidsm).
- Lewy body dementia (usually has visual hallucinations as a key characteristic, one can remember it as dementia that watches non-real bodies).
- Frontotemporal dementia (with early personality changes and disinhibition being key features of this disorder).
- Normal pressure hydrocephalus.
- Vitamin B12 deficiency.
- Epidural (acute) or subdural (subacute or chronic) hematomas.
- Cerebrovascular disease (Stroke, TIA).
- Delirium.
- Electrolyte abnormalities.
- Infections:
- Neurosyphilis.
- Meningitis.
- Encephalitis.
- Medication-induced memory loss: first generation anti-histamines, antiparkinsonian medications, TCA’s, antipsychotics, benzodiazepines, among others.
We hope that this post can help you better understand how to handle a case of memory loss or forgetfulness in your exam. Please, feel free to contact us should you have any comment or question by using the comments section below. Good luck with your studies.
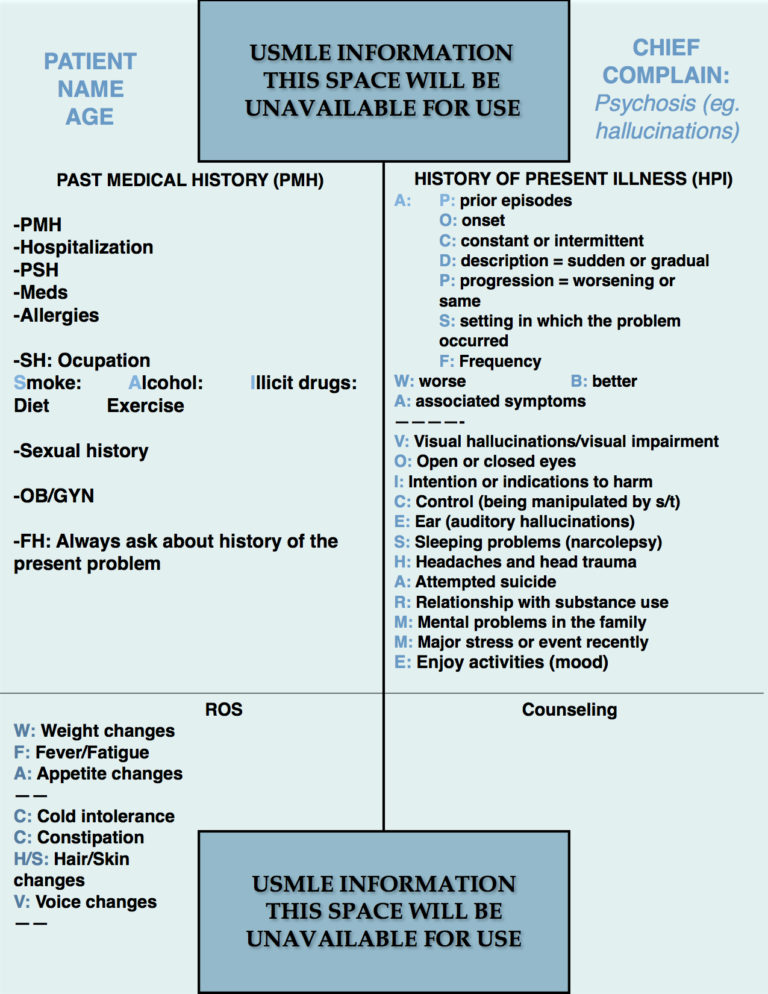
- Step 2 CS Blue Sheet Psychosis - 03/23/2018
- Step 2 CS Blue Sheet Memory Loss/Forgetfulness - 03/23/2018
- Step 2 CS Blue Sheet Shortness of Breath - 03/13/2018




Información muy importante ….. muchas gracias doctor