Step 2 CS Blue Sheet Dizziness Case:
Dizziness is a nonspecific term since it can be used by patients to describe different symptoms such as vertigo, unsteadiness, generalized weakness, syncope, presyncope, or falling. Therefore, the best first step in the history taking of these patients is asking them to further describe the “dizziness” they feel with other words or more specifically so that we can be sure of what are they experiencing.
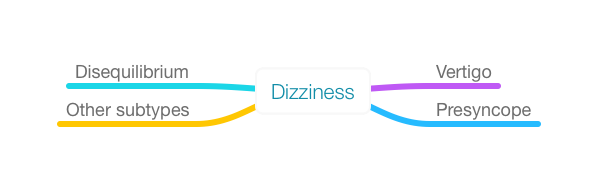
Subtypes of Dizziness:
There are 4 subtypes of dizziness:
1. Vertigo: Sensation that one or one’s surroundings are spinning or rotating.
2. Presyncope (lightheadedness): Sensation that one is about to pass out or fainting. It is mostly felt in the head.
3. Disequilibrium: Sensation of unsteadiness in the lower body that gets better when sitting or lying down. It is mostly felt in the lower limbs.
4. Other subtypes:
- Swimming or floating sensation: felt as if one is swimming in a pool.
- Feelings of dissociation from one’s body.
- Unspecified: Sometimes patients cannot specify what they feel when describing dizziness. It can also be described as a mixture of the different subtypes.
Dizziness is a tricky symptom because of this great personal variability of description and its nonspecific nature. One must keep in mind that dizziness must be identified as one of the different subtypes when possible for making an accurate differential diagnosis.
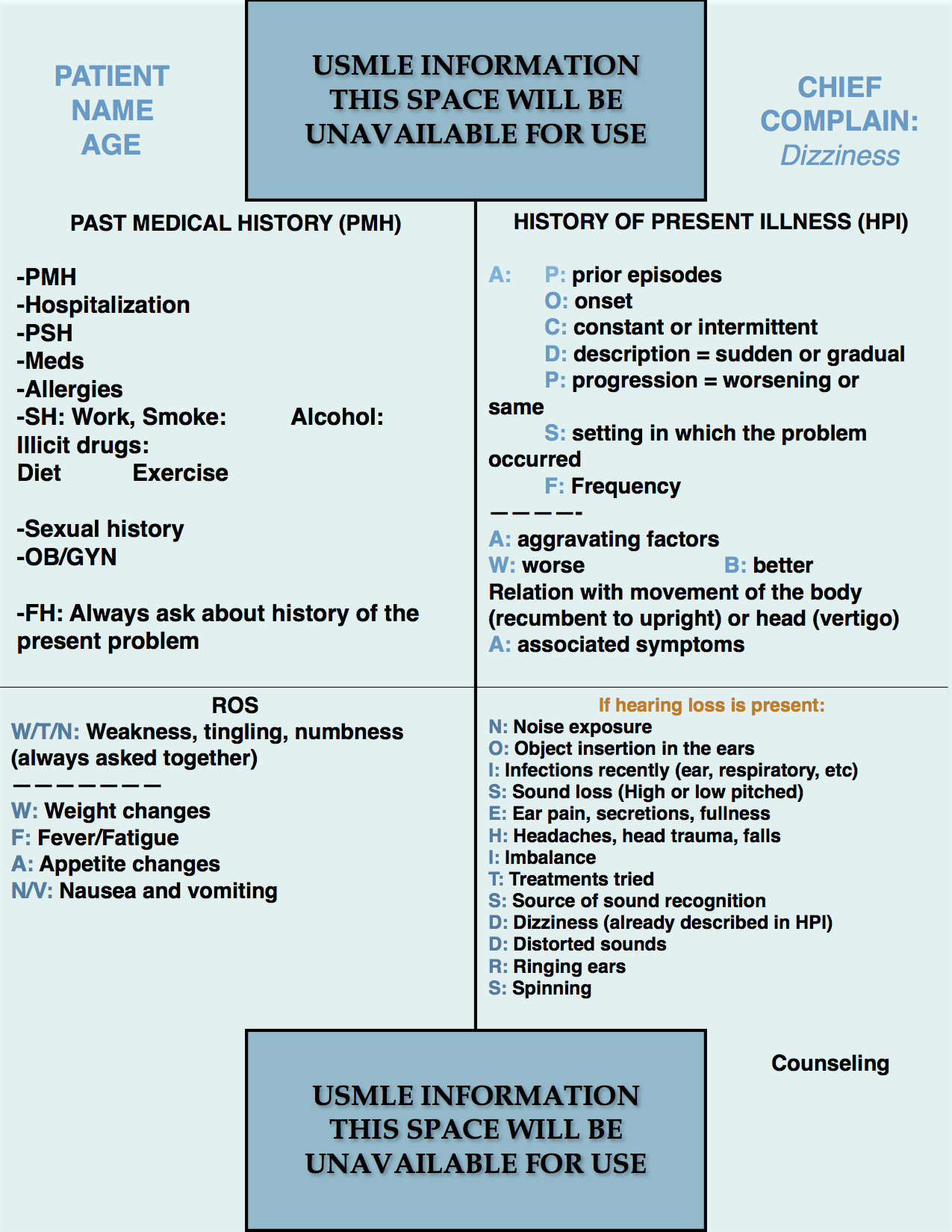
Next, let us review the blue sheet, physical exam, diagnostic studies, and differential diagnosis needed for a case of dizziness in the USMLE Step 2 CS exam:
Regardless of the subtype of dizziness, the blue sheet that one can use will not change. The past medical history section is similar to any other case with the exception of considering comorbidities such as cardiovascular risks for stroke or cerebellar disease, dementia, and other neurologic conditions. The past sexual history is important in a patient experiencing tabes dorsalis or neurosyphilis.
The history of present illness would be the same as any case without pain (ALICIA used in pain and AAA used without pain). Asking about nature (episodic vs constant) of the dizziness, duration of the episodes, and alleviating and worsening factors is essential.
The review of systems (ROS) should be directed towards the type of dizziness. However, since one does not know exactly the subtype until the patient encounter, the recommendation is to write the following mnemonics:
W/T/N: Weakness, numbness, tingling. These questions might be asked together almost in any case, mostly if there is a neurologic compromise of concern. It will recognize symptoms of stroke, peripheral nerve disease such as diabetic or others, etc.
WFA: Can be used for all cases. The mnemonic stands for:
W: Weight changes
F: Fever
A: Appetite changes
These three questions can help one to screen for constitutional symptoms, infections, psychological conditions such as major depression.
N/V: Nausea and vomiting usually are present in patients with dizziness, being more prominent in the vertigo subtype.
Finally, if the subtype of dizziness is vertigo, one can use the same mnemonic used for the hearing loss cases which is “Noise Hits The Ears adapted to NOISE HITS DD RS.”
N: Noise exposure
O: Object insertion in the ears
I: Infections recently (ear, respiratory, etc)
S: Sound loss (High or low-pitched)
E: Ear pain, secretions, fullness
H: Headaches, head trauma, falls
I: Imbalance
T: Treatments tried
S: Source of sound recognition
D: Dizziness (already described in the HPI)
D: Distorted sounds
R: Ringing Ears
S: Spinning
The reason why this mnemonic should be used is that vertigo has 2 major sources that are inner ear or cerebellar disorders. Therefore, it is key to screen for hearing problems in these patients.
PHYSICAL EXAMINATION
1. HEENT:
Inspection of the eyes for EOM, nystagmus, and pupillary reflexes.
Nystagmus may be simulated by the patients moving their eyes rapidly side to side or up and down when performing extraocular movements (EOM).
Fundoscopy.
Otoscopy for ear disorders.
Hearing tests: Weber and Rinne’s tests and whisper voice test (speaking to the patient from behind and both sides whispering a word to be repeated by the patient.
Oropharynx inspection when indicated.
2. Lungs:
Auscultation.
3. Heart:
Auscultation.
4. Neurologic:
Mental status: Alert and oriented to person, time, and place.
Cranial nerves 2-12.
Motor strength.
Sensory.
Deep tendon reflexes DTR’s.
Romberg sign and gait.
Cerebellar tests when appropriate (mostly with the disequilibrium subtype).
POSSIBLE DIAGNOSTIC STUDIES:
- Orthostatic vital signs (for orthostatic hypotension or syncope).
- Tilt test.
- VDRL/RPR (syphilis is associated with Meniere’s disease).
- Audiometry, brainstem auditory evoked potentials.
- Electronystagmography (for nystagmus assessment).
- MRI brain (when suspicion of masses or CNS disorders such as stroke).
DIFFERENTIAL DIAGNOSIS:
Think CNS, ear, and/or systemic disorders.
Vertigo subtype causes:
- Central vertigo: Stroke, TIA, vertebrobasilar insufficiency, multiple sclerosis, brain tumors, epilepsy, migraine.
- Peripheral vertigo causes: Benign positional paroxysmal vertigo (BPPV), Meniere’s disease, labyrinthitis, vestibulitis, acoustic neuroma, drug-induced ototoxicity (aspirin, aminoglycosides).
Other subtypes causes:
- Cardiovascular: Cardiac arrhythmias, orthostatic hypotension, anemia, hypovolemia, myocardial ischemia, valvular diseases, hypoxia, neurocardiogenic syncope, congestive heart failure.
- Neurologic:Stroke, TIA, vertebrobasilar insufficiency, multiple sclerosis, brain tumors, epilepsy, migraine.
- Psychiatric: Hyperventilation, anxiety, dissociative disorders.
- Others: Thyroid disorders, electrolyte abnormalities, sepsis, hypoglycemia (diabetic on insulin or sulfonylureas),
As one can notice, the differential diagnosis is very broad and that makes the subtype identification narrow the differential diagnosis. The data obtained from the patient during the encounter will make the differential diagnosis formulation more accurate and narrow.
We hope that this post can help you better understand how to handle a dizziness case in your exam. Please, feel free to contact us should you have any comment or question by using the comments section below. Good luck with your studies.
- Step 2 CS Blue Sheet Psychosis - 03/23/2018
- Step 2 CS Blue Sheet Memory Loss/Forgetfulness - 03/23/2018
- Step 2 CS Blue Sheet Shortness of Breath - 03/13/2018